|
| Memory loss results from disruption at any of these processes |
Forgetfulness and Memory Loss
Forgetfulness or failure to remember information, is a common complaint. All of us have at some time or the other forgotten to make that important call, to pick up some items from the store, an anniversary or birthday, or a colleague’s name. Students forget what they have “learnt” during exams. We often can’t remember where we have left our car keys, our wallet or that important document. Is it normal? And more importantly; when do we need to seek help?
Forgetfulness or memory loss and difficulty concentrating are common symptoms of mental health disorders. This is specially so in depression, anxiety disorders, ADHD (Attention Deficit Hyperactivity Disorder), and dementias as shown in the examples below.
A young working professional seeks help for increased forgetfulness and poor ability to focus at work. Further probing reveals decreased interest in doing things at work and home. She is also irritable, depressed and her sleep is disturbed. These symptoms of low mood can exist in the background of memory loss and problems with focus.
A student during exams has high anxiety causing memory loss. She cannot recall the answer to a certain question. She gets nervous. This causes her to make mistakes in the next question. She tends to panic; fail to recall what she studied. This vicious cycle is common in anxiety disorders and can manifest as problems with concentration, memory and forgetfulness.
An older person does not just forget the name of his neighbour (something that may happen to any of us); but also who she is. He has problems using money, and with shopping. Difficulties at work manifest towards the end of the career. Dementias affect the aged; cause memory loss and affect the context of the memory.
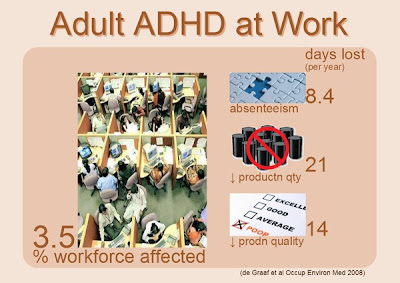
A young professional has problems organising and completing projects at work. There may be a history of attention and academic problems in school. Working memory gaps are common in this group. ADHD is a common cause of this problem in adults.
Memory Processing in the Brain
To understand further, it helps to know in brief how memory works. It is a 3 stage process- Encoding
- The stage when sounds, images and other sensations are given meaning is called encoding. Sensations are coded electrically for access by other brain areas. (We hear a catchy song from a new movie).
- Storage
- The process of association or tagging the input with other bits of data to make it persist. The song thus gets stored in our long term memory. Initially, the song remains for a very short while. At this point it is in our working or short term memory. It is encoded. However, we forget the song as the next scene unfolds on screen. The song is repeated at the end of the movie; someone hums the song as we leave the hall. The visuals of the song, and the feelings evoked, the fact that it was a famous actor, then reinforce the memory and makes it persist.
- Retrieval
- When we need to use this stored data, the brain fishes it out from its long term memory. The more the associations or tags we formed earlier, the more easily the brain can access the information.
Problems in memory can therefore occur at any of these stages. Many of these occur at the stage of encoding because we are simply not paying attention; and many other distractions are vying for our focus at the same time. (e.g checking our FB messages while studying). The brain does not multi-task, it can only do one thing at a time.
Repetition, rehearsal and organisation help in fixing and storage of long term memory. The more widespread and elaborate the connections, and the more data available about an input, the more the connections formed by the brain, and the easier it is for the brain to retrieve the information when required. Many cases of forgetting are due to retrieval failures. The information is there in long term memory but we are unable to access it. This is why we can recall certain things at a later date.
Depression affects memory in many ways. Being unable to concentrate is a symptom of depression. Repeated depressive thoughts also block the learning process through distraction. This affects the stage of encoding. Disturbed sleep which is a common symptom in depression hampers fixing into long term memory.
Forgetfulness is common in ADHD of adults. ADHD lowers the power to focus. The person is easily distracted. The attention span is reduced. This impairs short term or working memory. ADHD persists in up to 40% of aduts.
Anxiety gives rise to pointless thoughts (“my father will be so angry if I don't crack this exam”) which frustrates attempts to retrieve the matter learned. The anxiety provoking thoughts distract from the text which is being studied and impedes the encoding process.
In dementia there is destruction and loss of brain cells. Dementia blocks all stages of the memory and learning process. The process is not reversible.
Forgetfulness is common in ADHD of adults. ADHD lowers the power to focus. The person is easily distracted. The attention span is reduced. This impairs short term or working memory. ADHD persists in up to 40% of aduts.
Anxiety gives rise to pointless thoughts (“my father will be so angry if I don't crack this exam”) which frustrates attempts to retrieve the matter learned. The anxiety provoking thoughts distract from the text which is being studied and impedes the encoding process.
In dementia there is destruction and loss of brain cells. Dementia blocks all stages of the memory and learning process. The process is not reversible.
Forgetfulness and Memory Loss – when to seek help?
- When it affects our work, or the quality of our work
- When the failure to learn and recall affects our daily activities and functioning
- When there are also problems including sleep, appetite, inter-personal or behaviour changes.
- When it is strange - leaving keys in the fridge
- When it can harm - often leaving cooking burner on, leaving doors unlocked at night
In normal forgetfulness, the person may recall the memory when some cues are given. The memories were encoded, they just needed some reminder to access them. In clinical disorders resulting in memory loss the memories were never laid down in the first place, or the storage structures in the brain are destroyed. Access to these memories may not be possible.
References
- Brydges CR, Ozolnieks KL, Roberts G. Working memory - not processing speed - mediates fluid intelligence deficits associated with attention deficit/hyperactivity disorder symptoms. J Neuropsychol. 2015 Dec 31. doi: 10.1111/jnp.12096. [Epub ahead of print]