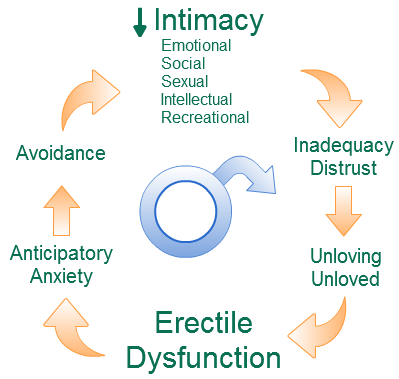
Rejecting an unwanted lover unceremoniously can be dangerous. Rejection sensitivity and aggression by the scorned male can have disastrous consequences. Last week a college girl was attacked with a sickle for doing so. The demographic profile of students at our clinic is probably a representation of the Pune student population. Many students feel socially and culturally alienated while having to cope on their own with minimal family support. Some have no one to express their feelings or thoughts to. A smile or other facial expressions from a classmate or a single phrase while watching a game are viewed as tokens of intimacy. Subsequent fantasising invests these facial expressions and interactions with an excessive significance. That the girl does not initiate or acknowledge further interaction is rationalised as shyness and considered a virtue, further embedding the myth of intimacy.
The concept of gender equality may be alien in the culture of the student. It comes as a great shock to the lover, when he gathers up his courage to proclaim his love only to find it discarded unceremoniously. His reaction will depend on his attachment style - the behavioural response to separation developed in childhood. Mostly he will withdraw further into his shell, but in some cases, especially when he is high on the personality characteristic of rejection sensitivity and has a fearful attachment style, he will harbour and act out thoughts of revenge.These vengeful thoughts smoulder unrecognised until they burst forth in as dramatic and unexpected action as the initial profession of love.
Rejecting an unwanted lover
Rejection sensitivity is always a concern when rejecting an unwanted lover. The independent modern woman needs to learn how to handle this situation without involving family or other third parties. Rejecting an unwanted lover can be considered as a form of breaking bad news. For this there is no better technique than the SPIKES 6-step protocol which is used to break bad news in medicine.- Setting
- Make sure there is privacy. No matter how startled you are by his profession of love, do not blurt out a summary dismissal in front of everyone. Stay in a public place, but take him to one side.
- Perception
- Ask him to clarify what he has just said, and what lead him to say that. This will help you to place him, if you haven't already done so.
- Invitation
- Ask whether you can tell him your point of view on the subject
- giving Knowledge
- Warning before giving the bad news helps the person process the information imparted without getting angry or feeling isolated. Start by saying "I am sorry to say that I don't feel that way". Don't be rude or excessively blunt Responses such as "who do you think you are?", "why should I have feelings for you?" or laughing contemptuously are bound to turn love into the other end of the stick - hate, especially if he is high on rejection sensitivity. Check his reactions and modify what you are saying so he can understand.
- Empathise
- Identify his emotion - sadness, anger, hurt. Closely monitor his facial expressions. Acknowledge it. "I can see that you are feeling hurt. Anyone in your position might feel like that".
- Strategy
- Discussing what comes next. Start from his Perception of the relationship to help vent his emotions. Deal with these Empathically, again the facial expressions are important. The goal should be to politely but firmly communicate "I don't feel that way" so "we cant take this any further, don't take this personally".
Reference
- Baile WF, Buckman R, Lenzi R, Glober G, Beale EA, Kudelka AP. SPIKES-A six-step protocol for delivering bad news: application to the patient with cancer. Oncologist. 2000;5(4):302-11.