Hi. I’m Jai. I’m 8 years old. This is my story. My doctor says I have an illness. I don’t feel sick. But I do know that grown-ups around me are annoyed with me most of the time. I’m constantly being told, “sit still’’, “stop dreaming”, “pay attention”. I can’t seem to be able to do just that.
In class, I seem to lose track of what the teacher says. I try to listen, I really do. I start doing what she says, then I notice the insect fluttering on the window pane, I see the boy in the row ahead tapping his fingers on the desk, the office boy walking down the corridor and the sound of laughter from the next classroom. I don’t realise I have left my seat till teacher tells me “Jai, return to your seat”.
My parents are frequently called to school to meet my class teacher. They are unhappy with my marks. They think I’m careless and lazy because I take all evening to do my homework. I tell my mother that I try hard. I feel sad and frustrated that she doesn’t understand or believe me. Some of the other children make fun of me specially when I can’t answer in class. Mostly, I haven’t heard the question. They don’t like to play with me as I get excited and can’t wait for my turn.
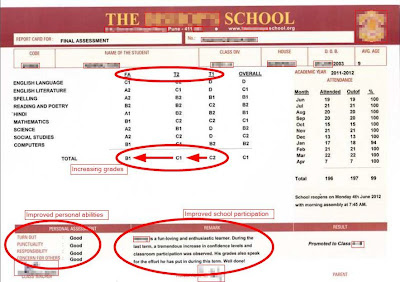
Things changed about 6 months back. My parents took me to a special doctor. The doctor seemed to understand that I was not being naughty or disobedient. He talked to me, looked at my exercise books and listened to my parents. He told my parents that I had an illness, ADHD. I needed medicines for treatment of ADHD to improve my focus and concentration. I also need structure and routine in my life. It was such a relief to know it was not my fault.
A lady at the doctor’s clinic gave me some puzzles and games to do. I liked her; she spoke slowly and clearly. She explained things one at a time and did not mind repeating herself when I did not get her the first time. She helped us draw up a time-table - we had such fun doing that because she made time for everything I want to do. Now I have a study time, a play time, TV time, all clearly written in the big chart I helped to make. It reminds me of what I have to do and gives me enough time to prepare for it. Mother says I sit quietly for longer periods. Teacher says I pay more attention and don’t disturb other kids in class. She is more patient with me too.
Understanding ADHD and Helping Me
Doctor says there are many children like me. Here’s what you can do to help me and others like me.- Help me focus. Make sure I’ve heard you and understood what you want me to do.
- I sometimes don’t realise I’ve left my seat. Please remind me to stop and think.
- I need structure and routine in my life.
- I need to know what comes next.
- Please give me time to adjust to any changes in my schedule.
- Please let me learn at my own pace, I get confused and make mistakes when you ask me to hurry up.
- Please give me instructions one step at a time. Make me repeat them.
- Please give me short work periods and small goals to start with.
- Please give me immediate feedback; did I do things the right way?
- Do give me praise even if I succeed only partially. Please don’t wait till I’m perfect.
- Don’t always find fault with me. Please praise me and reward me when I do something well.
Thank you for being patient with me.